What is Pancreatic Cancer?
The pancreas is an organ of the digestive system located deep in the upper part of the abdomen, behind the stomach and in front of the spine. The pancreas is only about 2 inches wide and 6 to 8 inches long, and sits horizontally across the abdomen. It is composed of 3 contiguous parts:
- The large, rounded portion of the gland is called the head. It is located on the right side of the abdomen and abutting the beginning of the small intestine, which is called the duodenum.
- The middle section, called the body, is tucked behind the stomach.
- The thin end of the pancreas, called the tail, is located on the left side of the abdomen, next to the spleen.
The pancreas is a glandular tissue comprised of two cell types:
- Exocrine – produces and secretes substances into a duct, which drains into the duodenum.
- Endocrine – produces and secretes substances into the blood tissue.
The exocrine tissue comprises 95% of the pancreas, and the endocrine tissue makes up the remaining 5% of the pancreas.
Exocrine glandular tissue produces pancreatic enzymes. These enzymes travel down the pancreatic duct and into the duodenum where they aid in the digestion of food. The endocrine glandular tissue of the pancreas produces hormones and releases them into the bloodstream. Two of these hormones—insulin and glucagon—help control blood sugar levels.
What is Cancer of the Pancreas?
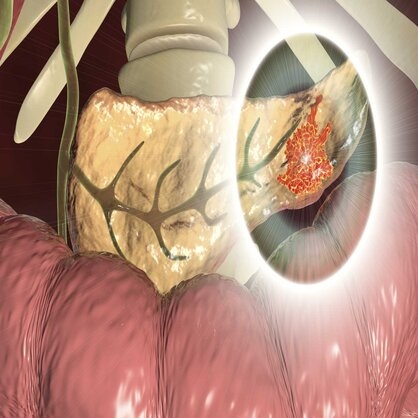
Pancreatic cancer develops when abnormal cells in the pancreas grow and divide out of control to form a tumor.
Because the pancreas lies deep in the abdomen, a doctor performing an examination on a patient would not be able to feel a pancreatic tumor. Pancreatic cancer has no early warning signs, and there are currently no effective screening tests. As a result, pancreatic cancer is usually discovered late. Often, the diagnosis is not made until the cancer has spread to other areas of the body (stage IV). However, research focused on better diagnostic tests and newer treatments provides a more optimistic future for patients diagnosed with pancreatic cancer. In fact, a blood test and better scans are in development.
Before 2030, pancreatic cancer is expected to be the second-leading cause of cancer-related deaths in the United States, second only to lung cancer.
Types of Pancreatic Cancer
It is important to distinguish between exocrine and endocrine tumors because each has different pancreatic signs and symptoms, is diagnosed using different tests, has different treatments and has different prognoses.
The most common type of pancreatic cancer, and the one we focus our research efforts on, arises from the exocrine cells and is called a pancreatic ductal adenocarcinoma (PDAC). These tumors are designated “ductal” because they microscopically form structures that resemble the pancreatic ducts. About two-thirds of all pancreatic cancers arise in the head of the pancreas. The remainder arise in the body and tail. These tumors are malignant, meaning they can invade nearby tissues and organs. Cancerous cells can also spread, or metastasize, through the blood and lymphatic systems to other parts of the body.
Tumors can also resemble the endocrine cells of the pancreas. These types of rare tumors are called islet cell tumors, pancreatic endocrine neoplasms, or pancreatic neuroendocrine tumors, are generally less aggressive and may be curable if detected early.
Precursors to Pancreatic Cancer
An understanding of the lesions that give rise to pancreatic cancer is important because many of these precursor lesions can be identified and removed before they cause pancreatic cancer. Some of these precursors form cysts, which are collections of fluid within the substance of the pancreas.
Pancreatic Cysts
Almost 3% of American adults have a pancreatic cyst. Improvements in imaging tests over the past decade have led to a significant increase in the number of patients found to have a cyst in their pancreas. Most of these cysts are harmless and can be safely watched and followed.
Intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs)
IPMNs and MCNs have been recognized as special types of cysts in the pancreas because they are precursor lesions that can later progress to invasive cancers if left untreated. Both IPMNs and MCNs are called “mucinous” because they produce large amounts of mucus. In the case of IPMNs, they can clog and enlarge the pancreatic duct.
IPMNs and MCNs are very different from most pancreatic tumors because they may be present for a long time without spreading. Surgical removal [link to new Surgery URL] is the treatment of choice for IPMN cysts that are at high risk of progression to invasive pancreatic cancer. However, doctors have to balance the risk of over-treating patients with harmless cysts with the benefit of removing a precancerous lesion. Many small IPMN and MCN cysts can safely be followed with annual surveillance imaging, most commonly using magnetic resonance imaging (MRI) scans.
Because it can be hard to tell which IPMNs and MCNs are precancerous and which are harmless, researchers have been studying them and their genetic makeup for new ways to determine which are more likely to progress to pancreatic cancer. Our researchers are actively developing new molecular tests to better classify pancreatic cysts.
Researchers at Johns Hopkins are making incredible progress in evaluating which cysts are likely to develop into pancreatic cancer, so only those patients with pre-cancerous cysts undergo surgical removal. They have identified a panel of molecular markers and clinical features that show promise for classifying pancreatic cysts and determining which cysts require surgery.
This panel has the potential to lower the number of unnecessary surgeries by an overwhelming 91%. This more specific panel of markers is likely to provide physicians with additional information to help them determine whether surgery or surveillance of the cyst(s) is the most appropriate course of action for their patients, based on the type of mutation they see in a particular cyst.
Using this data, they have developed the Comprehensive Cyst (CompCyst) test, which combines clinical, radiological, genetic and protein marker information to classify pancreatic cysts. Avoiding unnecessary pancreatic surgery is important, and this research on cysts is one step forward.

