A Timeline of Pancreatic Cancer Research Milestones
Led by Lustgarten
 The Lustgarten Foundation was born from a need for better treatment options and outcomes for pancreatic cancer patients and their families. Today, we are leading the industry by funding bold, innovative research with a clear vision of a future with pancreatic cancer cures. Together, we are transforming pancreatic cancer into a curable disease.
The Lustgarten Foundation was born from a need for better treatment options and outcomes for pancreatic cancer patients and their families. Today, we are leading the industry by funding bold, innovative research with a clear vision of a future with pancreatic cancer cures. Together, we are transforming pancreatic cancer into a curable disease.
Join us as we celebrate 25 years powered by science and push toward a hopeful future inspired by you.
1998

The Lustgarten Foundation was born from a need for better treatment options and outcomes for pancreatic cancer patients and their families. Today, we are leading the industry by funding bold, innovative research with a clear vision of a future with pancreatic cancer cures. Together, we are transforming pancreatic cancer into a curable disease.
1999

Michael Goggins, MD, who had just joined the Johns Hopkins faculty with an interest in developing tests to improve the early detection of pancreas cancer, receives a $300,000 award helping to launch his pancreatic cancer research career.
1999
Elizabeth Jaffee, MD, receives a $700,000 grant to progress her important work in immunotherapy for pancreatic cancer at Johns Hopkins.
2000

The National Cancer Institute (NCI) convenes the first Pancreatic Cancer Progress Review Group. Lustgarten plays a key role in developing the national agenda for pancreatic cancer research.
2002
David Tuveson, MD, PhD, develops the first mouse model of pancreatic cancer. This model remains in use today to test new pancreatic cancer therapies
2004
Researchers begin using a combination of screening technologies—CT scan and endoscopic imaging—to screen for pancreatic tumors in patients with a strong family history or genetic predisposition to pancreatic cancer. The goal is to identify cancers at early stages so they can be removed surgically and are potentially curable.
2006

Lustgarten creates a phase III research project with the NCI to support the Cancer of the Pancreas Screening (CAPS) study, led by Marcia Canto, MD, at Johns Hopkins. CAPS is the first multi-center national study to detect pancreatic cancer and its precursor lesions among individuals with an inherited risk for pancreatic cancer.
2008

Bert Vogelstein, MD, completes the Pancreatic Cancer Genome Project, funded by Lustgarten. This is the most comprehensive genetic sequencing for any cancer. The findings shed new light on the genetic complexity of pancreatic cancers, but also present many potential targets for new cancer treatments. The project is a Science Magazine Top Three “Breakthroughs of the Year.”
2010
A new study, published in Nature, shows many pancreatic tumors don’t become lethal until nearly 20 years after the first genetic changes appear, suggesting an opportunity for earlier diagnosis.
2011
Research published in The New England Journal of Medicine shows as compared with gemcitabine, FOLFIRINOX was associated with a survival advantage. FOLFIRINOX becomes an option for the treatment of patients with metastatic pancreatic cancer and good performance status.
2012

The Lustgarten Foundation establishes the Lustgarten Advancing Breakthrough Science (LABS) Program funding the Lustgarten Foundation Pancreatic Cancer Research Laboratory at Cold Spring Harbor Laboratory. The lab is led by David Tuveson, MD, PhD, who also takes the role as the Foundation’s Chief Scientist. In the years since establishing the program, Lustgarten has funded additional LABS at MIT, Dana-Farber Cancer Institute, Salk Institute and two at Johns Hopkins.
2013
A large phase III trial shows that treatment with the combination of two chemotherapy drugs—Abraxane and gemcitabine—is more effective than standard single-drug therapy for people with metastatic pancreatic cancer. This combination becomes the new standard of care as first-line treatment for patients with metastatic pancreatic cancer.
2015
Ipsen’s Onivyde® (irinotecan liposome injection) is approved by the FDA as a second-line treatment for metastatic pancreatic cancer patients who previously received gemcitabine.
2016
Let’s Win! Pancreatic Cancer, an affiliate of the Lustgarten Foundation, creates a novel website enabling a community of doctors, scientists and patients to share important information to help patients find support, treatment options and available clinical trials.
2017
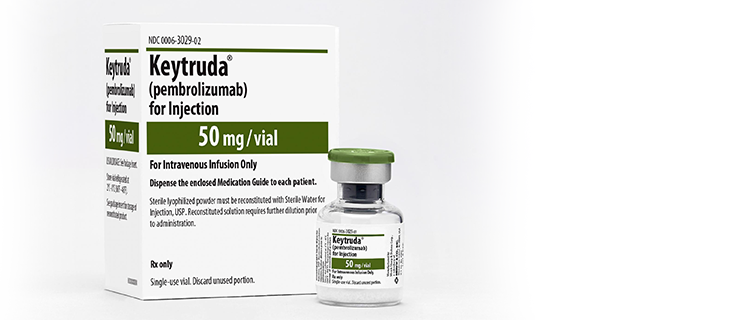
Merck’s Keytruda® (pembrolizumab) is approved by the FDA as the first immunotherapy for microsatellite instability-high (MSI-H) solid tumors. Lustgarten was a key funder of this important research. A small subset of pancreas cancer patients have MSI-H tumors and may be eligible for this medicine.
2017
Bert Vogelstein, MD, and his team at Johns Hopkins publish research in Science demonstrating two-thirds of cancer-causing mutations are random, unpredictable DNA copying “mistakes.” The remaining one-third of cases can be attributed to heredity or environmental factors, such as smoking and obesity.
2018

Building on a robust 5-year collaboration jointly funding more than 170 investigators who have started or completed 22 clinical trials, the Lustgarten Foundation and Stand Up To Cancer establish a formal strategic partnership, the Pancreatic Cancer Collective to drive research to improve outcomes for pancreatic cancer patients.
2018
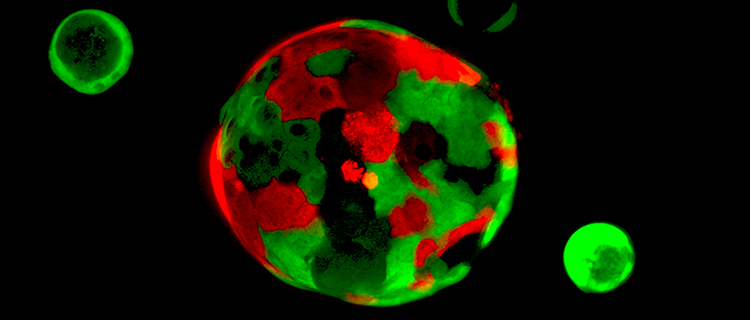
Funded by the Lustgarten Foundation and published in Cancer Discovery, the Tuveson Laboratory demonstrates pancreatic cancer organoids can predict therapeutic responses and facilitate precision medicine for patients with pancreatic cancer.
2018

Research published in The New England Journal of Medicine demonstrates treatment with modified FOLFIRINOX after pancreatic cancer surgery (adjuvant therapy) increases the time patients remain disease-free and overall survival compared with gemcitabine.
2018

FDA grants Breakthrough Device Designation for CancerSEEK, a liquid biopsy, for pancreatic and ovarian cancers—recognizing the unmet need for detection of these cancers and potentially speeding the availability of the test to patients. Lustgarten is a longtime funder of this research.
2018

James Allison, PhD, and Tasuka Honjo, MD, PhD, win the 2018 Nobel Prize in Physiology or Medicine for establishing an entirely new and potentially curative treatment strategy for cancer. Pioneers in the field of immunoncology, they win for demonstrating different strategies for inhibiting the brakes on the immune system.
2019
Elizabeth Jaffee, MD, Deputy Director, Sidney Kimmel Cancer Center at Johns Hopkins and Co-Director, the Gastrointestinal Cancers Program is appointed Lustgarten’s Chief Medical Advisor. A renowned immunotherapy researcher, Dr. Jaffee is leading the Foundation’s efforts to move new therapies from the lab to patients in the clinic.
2019

The FDA approves Astra Zeneca’s Lynparza® (olaparib), for the maintenance treatment of patients with changing germline BRCA-mutated (BRCA1 or BRCA2) metastatic pancreatic adenocarcinoma, whose disease has not progressed on at least 16 weeks of a first-line platinum- based chemotherapy regimen.
2019
The FDA approves the BRACAnalysis CDx test (Myriad Genetic Laboratories, Inc.) as a companion diagnostic for the selection of patients with pancreatic cancer for treatment with olaparib based on the identification of germline mutations.
2019

Lustgarten-funded researchers at Johns Hopkins, led by Elliot Fishman, MD, demonstrate computers can be trained to detect pancreatic tumors in CT scans, the first milestone toward employing artificial intelligence for earlier detection. Dr. Fishman’s work is reported in the American Journal of Roentgenology.
2020

Lustgarten launches the Dr. Robert F. Vizza Clinical Accelerator Initiative to employ cutting-edge biomarkers, shorten the time from clinical trial concept to trial launch and move therapies quickly from the lab to patients.
2020
The COMPASS study, published in Nature Genetics, analyzes the molecular subtypes of pancreatic cancer and identifies distinct subtypes of the disease with unique molecular properties that open new avenues for therapeutic development. The findings of this study are the building blocks for the Foundation’s ongoing PASS* (01) Trial. The trial employs organoids—3D models of an individual patient’s tumor—that can be grown in the lab, where multiple treatments can be tested on them.
* Pancreatic Adenocarcinoma Signature Stratification for Treatment
2021

Exact Sciences acquires Thrive Earlier Detection Corp., founded to commercialize CancerSEEK , a blood test capable of detecting multiple cancers, including pancreatic, early. Exact Sciences is developing new technologies to improve the test’s accuracy before beginning an 80,000-person registration trial seeking FDA approval.
2021
NCI SEER (Surveillance, Epidemiology, and End Results Program) data shows the survival rate for pancreatic cancer has more than doubled since 1998 to 10% today.
2022

The first-in-human vaccine trial to prevent pancreatic cancer in high-risk, healthy individuals, funded by Lustgarten and Stand Up To Cancer, opens at Johns Hopkins. The New York Times reports on vaccines to protect healthy people at high risk of developing cancer, noting the first vaccine with the hope of success is for individuals with a chance of developing pancreatic cancer.
2022

Positive results emerge from the first clinical trial using mRNA vaccines to treat post-surgical pancreatic cancer patients in combination with chemotherapy. Funded by Lustgarten and Stand Up To Cancer, each vaccine is personalized for the individual patient and contains neoantigens most likely to stimulate T cells. Trial results suggest the possibility of a more durable response and the feasibility of developing patient-specific, personalized vaccines in a clinically relevant timeframe. A larger phase 2 clinical trial is planned to confirm the results and make improvements to extend the effect to more participants.
5/24/23 Update:
Results published in Nature
2022

A groundbreaking study published in the Journal of Clinical Oncology shows surveillance programs for people at high risk of developing pancreatic cancer can detect precancerous conditions and cancers early. In the multicenter Cancer of Pancreas Screening-5 study, 1,461 high-risk individuals were enrolled at Johns Hopkins Medicine and seven other medical centers to undergo annual pancreatic imaging tests. Of these participants, 10 were diagnosed with pancreatic cancer. Seven were diagnosed with stage I disease and 1 with stage IIB. One participant was diagnosed four years after dropping out of recommended surveillance. Seven of these patients were alive after a median follow-up of 2.6 years.



