Organoids Accurately Predict Treatment Response of Pancreatic Cancer Patients
Topic: Announcement, Hide on Homepage, Press Releases
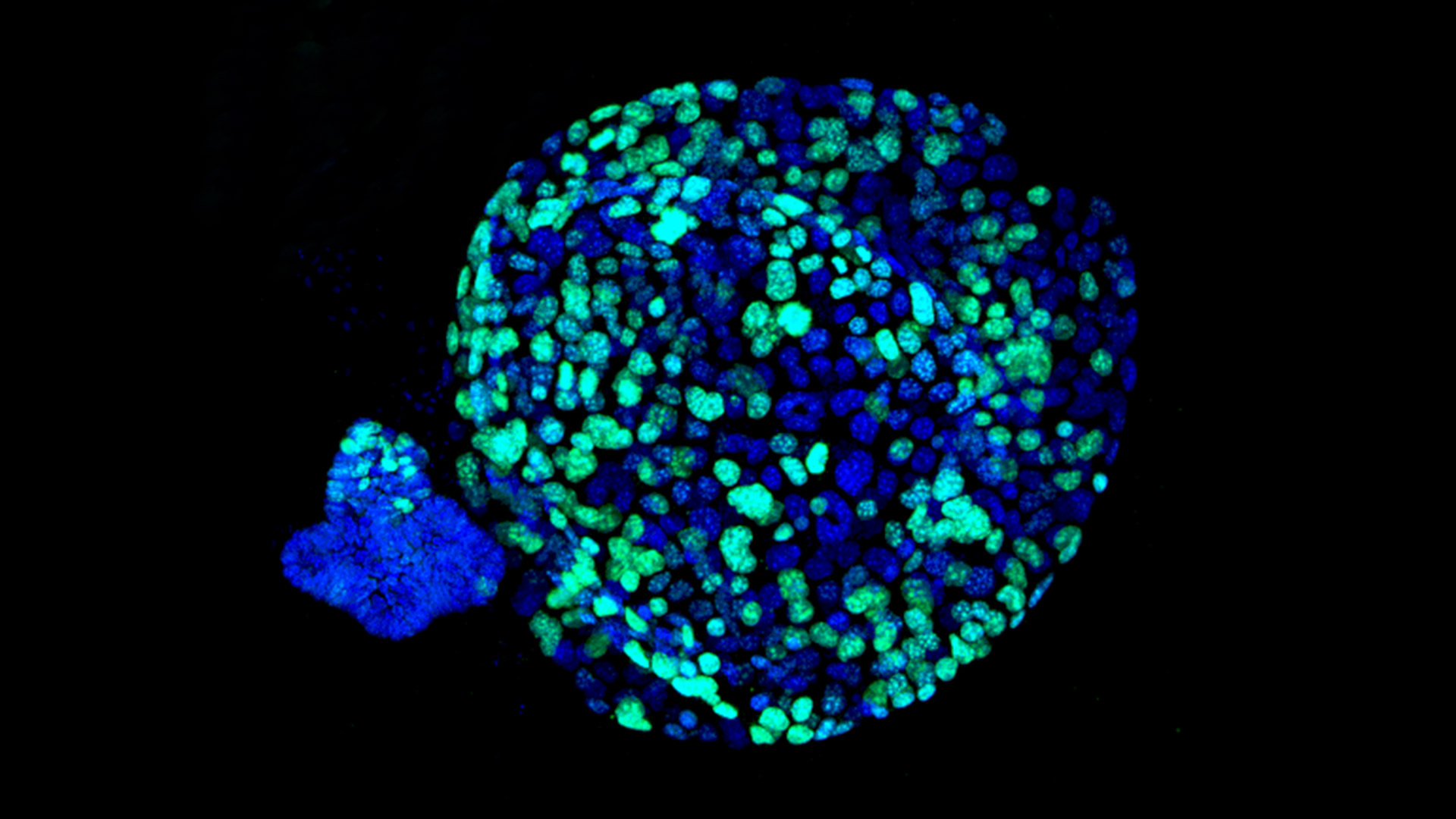
Lustgarten Foundation Dedicated Research Laboratory Developing Personalized Medicine Technology
Woodbury, NY (May 31, 2018) – Today in Cancer Discovery, an international team of researchers led by Dr. David Tuveson, Cold Spring Harbor Laboratory (CSHL) Professor and Chief Scientist of the Lustgarten Foundation, reports on results of 66 organoids derived from pancreatic ductal adenocarcinoma (PDAC) tumor specimens at various stages of the disease. The researchers demonstrated that the patient-derived organoids, which are three-dimensional hollow spheres of cells cultured from tumors, can quickly and accurately predict how patients with pancreatic cancer respond to a variety of treatments, facilitating a personalized medicine approach to the deadly disease.
“We’ve been able to identify an approach to prioritize treatment strategies for pancreas cancer patients, with the goal of giving them the best chance for survival and a good quality of life,” said Dr. Hervé Tiriac, a researcher in Dr. Tuveson’s lab and first author of the paper reporting the findings.
Several years ago, Dr. Tuveson recognized that organoids could significantly improve research into the disease. Aside from taking only as little as six weeks to grow, a major advantage of organoids is that they can be derived from patients with even very advanced pancreatic cancer, using tiny biopsies.
The researchers demonstrated that the organoids provide an effective personalized medicine “pharmacotyping,” or drug-testing, pipeline. To do this, the organoid from the patient’s cancer was cultured, and then used to test all possible standard-of-care drugs.
The team assessed RNA levels in individual organoids to determine gene signatures predictive of sensitivity to the five chemotherapies administered to pancreatic cancer patients. Three of these signatures correctly identified large numbers of patients who had responded to these drugs, and showed that responding patients lived much longer before the cancer progressed. Therefore, the signatures should in principle enable physicians to choose the correct chemotherapy for pancreatic cancer patients for first-line treatment. Since many of the organoids that did not respond well to chemotherapy were sensitive to a variety of investigational drugs, patients who lacked the sensitivity signatures might instead more quickly be treated with experimental agents.
Dr. Tuveson and his team plan to further refine the gene signatures through additional experiments, then test the genes’ ability to predict treatment sensitivity in clinical trials. In fact, Brian Wolpin, M.D., MPH, Director of the Hale Center for Pancreatic Cancer Research and of the Gastrointestinal Cancer Center at Dana-Farber Cancer Institute, is in the early stages of utilizing the organoid technology to identify new treatment options for patients with advanced pancreatic cancer.
“We have recently opened a protocol at Dana-Farber where patients with advanced pancreatic cancer can undergo a biopsy of their cancer for the generation of organoids. Once the organoids have grown sufficiently, we conduct drug screens to identify the vulnerabilities within a particular patient’s cancer,” Dr. Wolpin said. “We then deliver this information back to the treating oncologist to determine whether it can be useful in identifying new treatments for that patient. The effectiveness of this approach for patients remains to be demonstrated, but it is an example of how work being done in the laboratory can be applied to patient care in real time.
The Theodore W. Batterman Family Foundation Inc. partially supported this research.

